Course Syllabus
- Was ist GCP?
- Warum ist ICH GCP wichtig?
- Die Grundprinzipien der ICH GCP
- Zusätzliche Lerninhalte
- Dokumentation und Versionskontrolle
- Qualitätssicherung (QA)
- Wichtige Ressourcen
- Einführung
- Verantwortlichkeiten der zuständigen Behörde (CA)
- Verantwortlichkeiten der Ethikkommission (IEC)
- Aufklärung und Einwilligung der Probanden (ICF): Teil 1
- Aufklärung und Einwilligung der Probanden (ICF): Teil 2
- Zusammensetzung, Aufgaben, Arbeitsweise, Verfahren und Aufzeichnungen
- Einführung
- Verantwortlichkeiten des Prüfarztes
- Qualifikationen und Vereinbarungen des Prüfarztes
- Ausreichende Ressourcen
- Medizinische Versorgung der Studienteilnehmer: Teil 1
- Medizinische Versorgung der Studienteilnehmer: Teil 2
- Kommunikation mit IRB/IEC
- Einhaltung des Prüfplans
- Prüfpräparate (Investigational Medicinal Products)
- Randomisierungsverfahren und Entblindung
- Einwilligungserklärung der Studienteilnehmer: Teil 1
- Einwilligungserklärung der Studienteilnehmer: Teil 2 – Die Debatte über Einwilligungen
- Einwilligungserklärung der Studienteilnehmer: Teil 3 – Einwilligung bei Analphabetismus
- Einwilligungserklärung der Studienteilnehmer: Teil 4 – Einwilligung bei Minderjährigen und „nicht einwilligungsfähigen“ Personen
- Einwilligungserklärung der Studienteilnehmer: Teil 5 – Einwilligung bei urteilsunfähigen Probanden
- Einwilligungserklärung der Studienteilnehmer: Teil 6 – Aktualisierung der Einwilligung
- Aufzeichnungen und Berichte: Teil 1 – Einführung
- Aufzeichnungen und Berichte: Teil 2 – Studienordner
- Aufzeichnungen und Berichte: Teil 3 – Updates und Änderungen
- Aufzeichnungen und Berichte: Teil 4 – Quelldokumente
- Aufzeichnungen und Berichte: Teil 5 – Finanzinformationen
- Aufzeichnungen und Berichte: Teil 6 – Fallberichtformular (CRF)
- Aufzeichnungen und Berichte: Teil 7 – Erfassung von Probandendaten
- Vorzeitiger Abbruch einer Studie
- Fortschritts- und Abschlussberichte des Prüfarztes
- Archivierung
- Einführung
- Qualitätsmanagement: Teil 1
- Qualitätsmanagement: Teil 2
- Qualitätssicherung und Qualitätskontrolle (QA und QC): Einführung
- QA und QC: Standardarbeitsanweisungen (SOPs)
- QA und QC: Vereinbarungen & Verträge
- Auftragsforschungsinstitute (CROs)
- Studiendesign
- Studienmanagement, Datenmanagement und Dokumentation: Teil 1 – Forschungsmanagement
- Studienmanagement, Datenmanagement und Dokumentation: Teil 2
- Studienmanagement, Datenmanagement und Dokumentation: Teil 3
- Studienmanagement, Datenmanagement und Dokumentation: Teil 4 – Elektronische Datensysteme
- Studienmanagement, Datenmanagement und Dokumentation: Teil 5 – Aufbewahrung von Unterlagen
- Auswahl des Prüfarztes: Einführung
- Auswahl des Prüfarztes: Genehmigungen
- Auswahl des Prüfarztes: Verantwortlichkeiten
- Auswahl des Prüfarztes: Vergütung
- Finanzierung
- Anzeige/Einreichung bei den Aufsichtsbehörden
- Genehmigung durch die zuständige Behörde in der EU
- Bestätigung der Prüfung durch IRB/IEC
- Informationen zum Prüfpräparat (IMP)
- Herstellung, Verpackung, Kennzeichnung und Codierung der Prüfpräparate: Teil 1
- Herstellung, Verpackung, Kennzeichnung und Codierung der Prüfpräparate: Teil 2
- Lieferung und Handhabung der Prüfpräparate
- Zugriff auf Aufzeichnungen
- Audit und Inspektion
- Nichteinhaltung
- Vorzeitiger Abbruch oder Aussetzung einer Studie
- Prüfbericht/Studienbericht
- Multizentrische Studien
- Einführung
- Monitoring: Teil 1
- Monitoring: Teil 2 – Aufgaben des Monitors
- Monitoring: Teil 3 – Die Nachbeobachtungsvisite
- Monitoring: Teil 4 – Überprüfung des Prüfpräparats
- Monitoring: Teil 5 – Einhaltung von Prüfplan, Änderungen, SOPs und Leitlinien
- Monitoring: Teil 6 – Überprüfung der Einwilligungserklärung
- Monitoring: Teil 7 – Fallberichtformular (CRF) und Quelldokumente
- Monitoring: Teil 8 – Überprüfung der Probandendaten
- Monitoring: Teil 9 – Fehler
- Monitoring: Teil 10 – Abschluss des Monitoringbesuchs
- Monitoringbericht & Plan
- Qualitätsmanagement – Zentrales Monitoring
- Betrug und Fehlverhalten
- Einführung
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 1 – Unerwünschte Ereignisse (AEs)
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 2 – Schwerwiegende unerwünschte Ereignisse (SAE)
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 3 – Verdächtige, unerwartete, schwerwiegende unerwünschte Reaktionen
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 4 – Ereignisse von besonderem Interesse
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 5 – Periodische Sicherheitsberichte
- Berichte über unerwünschte Arzneimittelwirkungen: Teil 6
- Einführung
- Struktur und Inhalt des Protokolls
- Einführung
- Struktur und Inhalt der Prüferinformation
- Einführung
- Wesentliche Dokumente
- Archivierung
- Dokumente, die vor Studienbeginn vorliegen müssen
- Dokumente, die während der Studie vorliegen müssen
- Dokumente, die nach der Studie vorliegen müssen
- Einführung
- Was unterscheidet GCP in Deutschland von ICH-GCP?
- Prüfer und Prüfgruppen: Teil 1
- Prüfer und Prüfgruppen: Teil 2
- Prüfer und Prüfgruppen: Teil 3
- Antrags- und Genehmigungsverfahren
- Weitere Materialien
Our GCP certified customers


Good Clinical Practice (GCP) training is a vital educational programme designed to arm clinical trial professionals and researchers with essential knowledge about ethical and scientific standards. These standards are crucial for executing high-quality clinical trials. The training encompasses the globally recognised guidelines set forth by the International Council for Harmonisation (ICH).
The key objectives of GCP training include:
- Safeguarding the rights, safety, and welfare of human participants
- Upholding the accuracy and reliability of data collected during clinical trials
- Fostering uniform, top-tier practices across all facets of clinical research
The Whitehall Training Good Clinical Practice Course thoroughly explores these critical areas, offering learners a robust grounding in both the theoretical principles and practical applications of Good Clinical Practice.
For those involved in clinical trials research, obtaining GCP certification is essential.
If you're keen to broaden your knowledge of the field, GCP certification offers significant benefits, including:
- Alignment with global regulatory requirements
- Bolstering the integrity and standard of research
- Safeguarding the rights and well-being of study participants
- Expanding career opportunities within clinical research
Our Whitehall Training Good Clinical Practice Course not only results in certification but also imparts practical knowledge for effectively implementing GCP principles in your day-to-day work.
Good Clinical Practice (GCP) certification is crucial for numerous roles within the field of clinical research:
- Lead and Co-Investigators: Those who bear primary responsibility for conducting trials at research locations.
- Research Support Teams: This includes study coordinators, clinical research nurses, and other on-site personnel integral to trial operations.
- Trial Sponsors and Research Organisations: Individuals overseeing the planning, commencement, and documentation of clinical studies.
- Oversight Bodies: Officials tasked with monitoring and assessing trial compliance with regulations.
- Ethics Committees and Review Boards: Members involved in the evaluation and approval of trial protocols.
- University and Research Centre Staff: Those ensuring that institutional research aligns with global standards.
- Researchers Funded by National Bodies: All staff and investigators participating in nationally funded clinical trials.
The Whitehall Training Good Clinical Practice Course is designed to meet the needs of this broad spectrum of professionals, offering both general GCP principles and role-specific guidance.
Additionally, our course proves beneficial for individuals aiming to enhance their research capabilities and refine their clinical trial management skills.
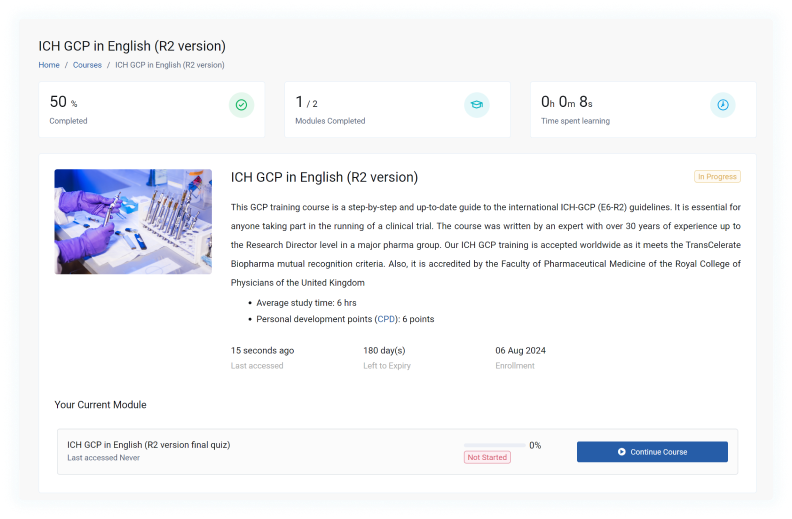
Our Good Clinical Practice (GCP) course thoroughly covers the ICH-GCP (E6-R2) international guidelines, ensuring you meet the training requirements for participation in global clinical trials. We offer this comprehensive training in multiple languages to cater to a diverse audience.
This course serves as a contemporary, step-by-step guide to the ICH-GCP (E6-R2) guidelines, making it an indispensable resource for anyone involved in clinical trial management. The content has been meticulously crafted by an industry veteran with over three decades of experience, including a tenure as Research Director at a prominent pharmaceutical company.
We're proud to have received accreditation from the Faculty of Pharmaceutical Medicine of the Royal College of Physicians of the United Kingdom, underscoring the quality and relevance of our course material. To accommodate our international learners, we've made the course available in ten languages, including English, German, Bulgarian, French, Italian, Japanese, Polish, Portuguese, Russian and Spanish.
Understanding the importance of regional regulatory frameworks, we've developed tailored versions of this course for Australia, the UK, the US, France, Germany and Latin America. These localised editions ensure that participants receive training that's directly applicable to their specific regulatory environment.
Our course boasts a user-friendly, visually engaging format that facilitates easy cross-referencing with the ICH-GCP E6 document. Drawing from the author's extensive practical experience, it offers valuable insights into the real-world application of GCP principles. As an added benefit, participants can earn 6 CPD points upon successful completion of the course.
Indeed, our GCP course has received certification from a prestigious body. The Faculty of Pharmaceutical Medicine at the Royal College of Physicians has given their seal of approval to our programme. This organisation is well-regarded as the professional membership body for pharmaceutical physicians in the United Kingdom and has been establishing stringent research standards since 1989.
The certification from such a respected institution demonstrates that our course meets exacting industry and academic criteria. As a result, when you complete our GCP course, you'll receive a qualification that is widely acknowledged and valued within the field.
Several factors influence the cost of GCP training:
- Official endorsements: Has the course received approval from recognised bodies?
- International compliance: Does the training fulfil ICH standards, allowing participation in global clinical studies?
- Content relevance: Is the material current and authored by industry professionals?
- Duration of availability: For how long can students access the course materials?
At £79, our Whitehall Training GCP course offers excellent value due to:
- Endorsement: The Royal College of Physicians has accredited the course, awarding 6 CPD points.
- Global acceptance: Our training adheres to ICH E6(R2) guidelines, enabling involvement in international clinical trials.
- Expert-crafted content: Lucy Parker, our GCP specialist with over 10 years' experience leading research in major institutions like the NHS, has developed the course material.
- Ongoing access: We support continuous professional development by providing unlimited access to course resources.
For group bookings, we offer a 10% discount on purchases of 5 licences at checkout. If you're interested in larger group discounts, please contact our team for a tailored quote.
Whilst some no-cost GCP training alternatives exist, they typically come with several drawbacks:
- The content may be subpar (lacking accreditation) and not up-to-date
- They often fail to provide official certification, which is essential for conducting clinical research
These free options might serve as a rudimentary introduction to GCP principles for those merely seeking a basic overview. However, they generally fall short of meeting the stringent requirements necessary for professional development in clinical research.
Whitehall Training's Good Clinical Practice Course, on the other hand, offers comprehensive, accredited training that equips learners with the knowledge and certification required to actively participate in clinical trials. Our course ensures you're fully prepared and compliant with current GCP standards, providing a valuable investment in your professional growth and capabilities in the field of clinical research.
Our GCP course offers an in-depth exploration of the crucial principles and practices necessary for executing ethical and scientifically rigorous clinical trials. With a curriculum that spans from basic concepts to more complex topics, our programme caters to learners across all experience levels.
The course delves into several vital areas, including:
- The historical context and core tenets of GCP
- Defining the duties of investigators, sponsors, and monitors
- Navigating ethical dilemmas and consent procedures
- Crafting and following study protocols
- Managing safety reports and adverse incidents
- Upholding data quality and integrity
- Addressing regulatory obligations and authority interactions
- Maintaining essential records and documentation
- Proper handling of investigational medicinal products
- Best practices in site management and monitoring
We've designed our training to be both engaging and effective, utilising a variety of interactive e-learning techniques:
- Comprehensive educational material
- Authentic case studies and situational analyses
- Engaging knowledge assessments and quizzes
- Practical illustrations and industry-leading practices
- Chances for personal reflection and practical application
This multifaceted approach ensures that participants not only absorb the information but can also apply it effectively in real-world clinical research settings.
Acquiring your Good Clinical Practice certificate is a simple two-phase process:
- Work through our engaging, interactive educational content to complete the learning component.
- Take the online final assessment.
Feeling apprehensive about the GCP test? There's no need to worry. The examination is merely a necessary step to confirm your readiness for research participation. Should you not pass on your first attempt, you can easily revisit our comprehensive resource library to reinforce your understanding of any areas that need improvement, and then have another go at the exam.
Our Good Clinical Practice course is structured to ensure participants not only absorb the material but can effectively implement it in real-world clinical research environments. To achieve this, we've incorporated a variety of evaluation methods throughout the learning journey:
- Continuous Evaluation: As learners progress through each module, they encounter interactive challenges and practical scenarios. These serve to reinforce crucial concepts and provide immediate feedback on comprehension.
- Comprehensive Final Assessment: The course concludes with an in-depth examination that thoroughly evaluates the learner's understanding of GCP principles and their practical application. This assessment covers all key areas explored in the course, including:
- Ethical frameworks in clinical studies
- Regulatory compliance and adherence
- Key roles and their responsibilities in clinical trials
- Ensuring data integrity and managing quality
- Handling adverse events and safety reporting
Real-world Application: The final assessment includes questions designed to test how well learners can apply GCP principles to lifelike clinical trial situations.
To ensure all participants are thoroughly prepared for their role in clinical trials, successfully completing the final assessment is a requirement for obtaining GCP certification.
Recognising that everyone learns at their own pace, learners can attempt the final assessment as many times as needed. This approach ensures that all participants can achieve the necessary level of understanding to become GCP qualified.
Our Good Clinical Practice (GCP) course is crafted to cater to a diverse array of professionals engaged in clinical research. Whilst prior knowledge of clinical research can be advantageous, it isn’t essential. We’ve thoughtfully structured the content to suit varying degrees of experience and different roles within the clinical trial field.
This training proves especially beneficial for:
- Those coordinating clinical research
- Lead investigators and their supporting team
- Nurses specialising in research
- Individuals managing clinical trials
- Professionals handling data and biostatistics
- Experts in regulatory affairs
- Specialists in quality assurance
- Members serving on ethics committees
- Pharmacists participating in clinical trials
- Personnel from sponsors and Contract Research Organisations (CROs)
Whether you’re taking your first steps in clinical research or seeking to update your existing knowledge, our course offers a thorough exploration of GCP principles and their real-world application. We’ve designed it to be accessible and informative, regardless of your current level of expertise in the field.
Yes, our Good Clinical Practice (GCP) course is entirely web-based, providing learners with unparalleled convenience and adaptability. This digital format offers numerous benefits:
- Personalised learning speed: Students can navigate the course content at their own rhythm, aligning with their unique learning preferences and timetables. This approach enables a more thorough interaction with the material, free from the constraints often associated with traditional classroom settings.
- Round-the-clock availability: The course can be accessed at any time, from any internet-enabled device. Whether you’re at your workplace, in the comfort of your home, or on the move, the course materials are always within reach.
The ICH is a worldwide organisation that develops guidelines for pharmaceutical research and development, with Good Clinical Practice (GCP) being a key focus. Here are some important facts about ICH:
- It unites regulatory bodies and pharmaceutical industry experts.
- The ICH establishes globally recognised benchmarks for clinical trials.
- Their GCP guidelines aim to safeguard trial participants and ensure data reliability.
- These guidelines undergo regular updates, with ICH GCP E6(R2) being the most recent iteration.
Compliance with ICH guidelines is essential for conducting legitimate clinical trials. This is precisely why we’ve created our comprehensive GCP course. It meticulously covers all 13 fundamental ICH GCP principles, equipping you with the knowledge to carry out research that meets international standards.
ICH Good Clinical Practice E6 (R2) represents the latest version of the Good Clinical Practice guidelines, published in 2016 by the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. This update marks a substantial progression in GCP standards, adapting to the evolving nature of clinical research.
It’s essential for clinical research professionals to be well-versed in ICH GCP E6 (R2) for several reasons:
- It sets the current worldwide benchmark for ethically and scientifically robust clinical trial execution.
- Regulatory bodies across the globe often mandate adherence to these guidelines.
- It plays a vital role in safeguarding human participants and ensuring the integrity of trial results.
- Many research institutions and trial sponsors expect their teams and collaborators to be knowledgeable about and follow these updated guidelines.
The Whitehall Training Good Clinical Practice Course offers comprehensive coverage of ICH GCP E6 (R2). This ensures that learners gain a thorough understanding of these revised guidelines and can effectively implement them in their clinical research roles.
The International Council for Harmonisation's Good Clinical Practice (ICH GCP) guidelines are underpinned by 13 essential principles that establish the ethical and scientific benchmarks for clinical research. These crucial tenets encompass:
- Upholding ethical standards
- Ensuring benefits surpass potential risks
- Safeguarding participants' rights and wellbeing
- Providing comprehensive supporting evidence
- Developing protocols based on sound scientific principles
- Obtaining approval from Institutional Review Boards or Independent Ethics Committees
- Ensuring oversight by qualified medical professionals
- Engaging investigators with appropriate qualifications
- Securing informed consent from participants
- Maintaining precise records and reporting
- Preserving confidentiality
- Adhering to good manufacturing practices for investigational products
- Implementing robust quality assurance systems
Whitehall Training's Good Clinical Practice Course offers comprehensive instruction on these principles, equipping you with the knowledge to effectively implement them in practical clinical research scenarios. Our course is designed to give you a thorough understanding of how these principles shape the landscape of clinical trials and research.