Course Syllabus
- The History of GCP: Part 1 – What is Good Clinical Practice?
- The History of GCP: Part 2 - The Nuremburg Code
- The History of GCP: Part 3 - The Declaration of Helsinki
- The History of GCP: Part 4 - The International Conference on Harmonisation (ICH)
- The History of GCP: Part 5 - E6(R2)
- What is GCP?
- Why should we have GCP? (A quick quiz)
- The Basic Principles of FDA and ICH GCP: Part 1
- The Basic Principles of FDA and ICH GCP: Part 2
- The Basic Principles of FDA and ICH GCP: Part 3
- The Basic Principles of FDA and ICH GCP: Part 4
- The Basic Principles of FDA and ICH GCP: Part 5
- The Basic Principles of FDA and ICH GCP: Part 6
- The 13 Basic Principles of ICH GCP: Part 1
- The 13 Basic Principles of ICH GCP: Part 2
- The 13 Basic Principles of ICH GCP: Part 3
- Key ICH Guidelines listed on the FDA’s website
- Compliance Guidance Manuals
- Certificate of Confidentiality
- FDA Inspections: Part 1
- FDA Inspections: Part 2
- FDA Inspections: Part 3 - The FDA's BIMO Program
- US/EMEA GCP Inspection Agreement
- FDA GCP Compliance
- Impact of ICH GCP in the US
- FDA Acceptance of Foreign Studies: Part 1
- FDA Acceptance of Foreign Studies: Part 2
- FDA Acceptance of Foreign Studies: Part 3
- FDA Acceptance of Foreign Studies: Part 4
- Some General Points
- FDA GCP Regulation: Part 1
- FDA GCP Regulation: Part 2
- Important Practical Considerations: Part 1
- Important Practical Considerations: Part 2
- Other Resources
- Introduction to GCP - Webinar
- Introduction
- GCP During the Pandemic
- Responsibilities of the CA
- Responsibility of the IRB/IEC: Part 1
- Responsibility of the IRB/IEC: Part 2
- Responsibility of the IRB/IEC: Part 3
- Subject Informed Consent Forms (ICF): Part 1
- Subject Informed Consent Forms (ICF): Part 2
- Subject Informed Consent Forms (ICF): Part 3
- Subject Informed Consent Forms (ICF): Part 4
- Subject Informed Consent Forms (ICF): Part 5
- Subject Informed Consent Forms (ICF): Part 6
- IRB/IEC Composition, Functions, Operations, Procedures and Records: Part 1
- IRB/IEC Composition, Functions, Operations, Procedures and Records: Part 2
- IRB/IEC interactions with Sponsors and Investigators
- FDA’s IRB requirements: Part 1
- FDA’s IRB requirements: Part 2
- FDA’s IRB requirements: Part 3 – Structure
- FDA’s IRB requirements: Part 4 - Function
- FDA’s IRB requirements: Part 5
- Exceptions to Requirement for Obtaining Informed Consent
- Revised guidance on reporting IRB non-compliance: Part 1
- OHRP Reporting Guidance I
- Revised guidance on reporting IRB non-compliance: Part 2
- OHRP Reporting Guidance II
- Revised guidance on reporting IRB non-compliance: Part 3 - OHRP Reporting Guidance III
- Revised guidance on reporting IRB non-compliance: Part 4
- Revised guidance on reporting IRB non-compliance: Part 5
- Revised guidance on reporting IRB non-compliance: Part 6
- Revised guidance on reporting IRB non-compliance: Part 7
- Introduction
- What is an Investigator?
- FDA Investigator Responsibilities: Part 1
- FDA Investigator Responsibilities: Part 2
- FDA Investigator Responsibilities: Part 3
- FDA Investigator Responsibilities: Part 4
- Selecting Investigators and Monitors
- Recordkeeping and Record Retention: Part 1
- Recordkeeping and Record Retention: Part 2
- Disposition of Investigational Drug: Part 1
- Disposition of Investigational Drug: Part 2
- Control of the Investigational Drug: Part 1
- Control of the Investigational Drug: Part 2
- Investigator Records and Reports: Part 1 - Trial Master File
- Investigator Records and Reports: Part 2 - Trial Master File
- Investigator Records and Reports: Part 3 - Trial Master File
- Investigator Records and Reports: Part 4 - Study Site Files I
- Investigator Records and Reports: Part 5 - Study Site Files II
- Investigator Records and Reports: Part 6 - Source Documents I
- Investigator Records and Reports: Part 7 - Source Documents II
- Investigator Records and Reports: Part 8 - Financial Information and Contracts I
- Investigator Records and Reports: Part 9 - Financial Information and Contracts II
- Investigator Records and Reports: Part 10 - Financial Information and Contracts III
- Investigator Records and Reports: Part 11 - The Case Record Form (CRF)
- Investigator Records and Reports: Part 12 - Recording Subject Data
- Investigator Records and Reports: Part 13 - Recording Subject Data
- Investigator Records and Reports: Part 14 - Progress Reports and Final Report(s) by Investigator
- Investigator Records and Reports: Part 15 - Progress Reports and Final Report(s) by Investigator
- Investigator Records and Reports: Part 16 - Safety Reports
- Investigator Records and Reports: Part 17 - Assurance of IRB review
- Investigator Records and Reports: Part 18 - Inspection of investigator's records and reports
- Investigator Records and Reports: Part 19 - Handling of controlled substances
- Disqualification of a Clinical Investigator: Part 1
- Disqualification of a Clinical Investigator: Part 2
- Disqualification of a Clinical Investigator: Part 3 - Actions upon disqualification
- Disqualification of a Clinical Investigator: Part 4 - Disclosure of disqualification actions
- Disqualification of a Clinical Investigator: Part 5 – Information Sheet
- Disqualification of a Clinical Investigator: Part 6 - Reinstatement of a disqualified investigator
- Disqualification of a Clinical Investigator: Part 7 - Unreliable data I
- Disqualification of a Clinical Investigator: Part 8 - Unreliable data II
- Ineligible Patients
- Adequate Resources
- Medical Care of Trial Subjects: Part 1
- Medical Care of Trial Subjects: Part 2
- Communication with IRB/IEC
- Compliance with the Protocol: Part 1
- Compliance with the Protocol: Part 2
- Randomization Procedures and Un-blinding: Part 1
- Randomization Procedures and Un-blinding: Part 2
- Informed Consent of Trial Subjects: Part 1
- Informed Consent of Trial Subjects: Part 2
- Informed Consent of Trial Subjects: Part 3 - The Consent Discussion
- Informed Consent of Trial Subjects: Part 4 - Subjects who cannot read or write
- Informed Consent of Trial Subjects: Part 5 - Consenting minors and mentally incompetent subjects
- Informed Consent of Trial Subjects: Part 6 - Consenting Incapacitated Subjects
- Informed Consent of Trial Subjects: Part 7 - Updating Consent
- Premature Termination or Suspension of a Trial: Part 1
- Premature Termination or Suspension of a Trial: Part 2
- Introduction
- ICH Sponsor Responsibilities
- FDA-Specific Sponsor Responsibilities: Part 1
- FDA-Specific Sponsor Responsibilities: Part 2
- FDA-Specific Sponsor Responsibilities: Part 3
- FDA-Specific Sponsor Responsibilities: Part 4 - Form FDA 1572
- FDA-Specific Sponsor Responsibilities: Part 5
- FDA-Specific Sponsor Responsibilities: Part 6 - Further considerations
- Quality Management: Part 1
- Quality Management: Part 2
- Quality Management: Part 3
- QA and QC (Quality Assurance and Quality Control): Part 1
- QA and QC (Quality Assurance and Quality Control): Part 2 – SOPs (Standard Operating Procedures)
- QA and QC (Quality Assurance and Quality Control): Part 3 - Agreements and Contracts I
- QA and QC (Quality Assurance and Quality Control): Part 4 - Agreements and Contracts II
- Working with Contract Research Organizations (CROs): Part 1
- Working with Contract Research Organizations (CROs): Part 2
- Medical Expertise
- Trial Design: Part 1
- Trial Design: Part 2
- Enrichment strategies to support approval of drugs / Personalized Medicine development: Part 1
- Enrichment strategies to support approval of drugs / Personalized Medicine development: Part 2
- Trial Management: Part 1
- Trial Management: Part 2
- Trial Management: Part 3 - Data Management
- Trial Management: Part 4 - Electronic Data Systems I
- Trial Management: Part 5 - Electronic Data Systems II
- Trial Management: Part 6 - Electronic Data Systems III
- Trial Management: Part 7 - Electronic Data Systems IV
- Trial Management: Part 8 - Electronic Source Data I
- Trial Management: Part 9 - Electronic Source Data II
- Trial Management: Part 10 - Electronic Source Data III
- Trial Management: Part 11 - Record Keeping
- Trial Management: Part 12 - Record Keeping for FDA Inspections
- Trial Management: Part 13 - Record Keeping & Record Retention
- Trial Management: Part 14 - Record Keeping & Record Retention II
- Selecting Investigators: Part 1
- Selecting Investigators: Part 2
- Selecting Investigators: Part 3 – Resources
- Selecting Investigators: Part 4 - Resources
- Selecting Investigators: Part 5 - Permissions
- Allocation of Responsibilities
- Compensation to Subjects and Investigators: Part 1
- Compensation to Subjects and Investigators: Part 2
- Financing: Part 1
- Financing: Part 2
- Financing: Part 3 - The Physician Payment Sunshine Act
- Financing: Part 4 - The Physician Payment Sunshine Act
- Financing: Part 5 - The Physician Payment Sunshine Act
- Notification/Submission to FDA/CA
- Investigational New Drug (IND) Application: Part 1 - When an IND is required
- Investigational New Drug (IND) Application: Part 2 - Types of IND
- Investigational New Drug (IND) Application: Part 3
- Confirmation of Review by IRB/IEC
- Information on IP
- Manufacturing, Packaging, Labeling, and Coding IMP: Part 1
- Manufacturing, Packaging, Labeling, and Coding IMP: Part 2
- Supplying and Handling Investigational Products
- Record Access
- Adverse Drug Reaction Reporting: Part 1
- Adverse Drug Reaction Reporting: Part 2
- Monitoring Trial Progress
- Audit: Part 1
- Audit: Part 2
- Noncompliance: Part 1
- Premature Termination or Suspension of a Trial: Part 1
- Clinical Trial/Study Reports
- Multicenter Trials
- Enhancing the Diversity of Clinical Trial Populations
- Compensation When Things Go Wrong : Part 1 - The TeGenero Incident
- Compensation When Things Go Wrong: Part 2
- Introduction
- FDA's Guidance on Risk-Based Monitoring: Part 1
- FDA's Guidance on Risk-Based Monitoring: Part 2
- FDA's Guidance on Risk-Based Monitoring: Part 3
- FDA's Guidance on Risk-Based Monitoring: Part 4
- FDA's Guidance on Risk-Based Monitoring: Part 5
- FDA's Guidance on Risk-Based Monitoring: Part 6
- Monitor’s Responsibilities
- The Monitoring Visit: Part 1
- Informed Consent: Part 1
- Electronic Informed Consent: Part 1
- Tips for Regulatory Inspections (Common Findings)
- Verifying IP/IMP: Part 1
- Complying with the Protocol, Amendments, SOP and Guidance: Part 1
- The Case Record Form (CRF) and Source Documents: Part 1
- Electronic Source Data in Clinical Investigations: Part 1
- Errors in CRFs
- Closing out the Monitoring Visit: Part 1
- The Monitoring Report & Plan: Part 1
- Fraud and Misconduct: Part 1
- Fraud and Misconduct: Part 2 - The KETEK case
- Introduction: Part 1
- Sponsor and Investigator Responsibility Decision Tree
- Adverse Events
- Suspected Adverse Reactions
- Serious Adverse Events: Part 1
- Adverse Events of Special Interest
- IND Safety Reports
- Submission of IND Safety Reports: Part 1
- Reporting Results from Foreign Studies
- FDA Guidance for Safety Reporting: Part 1
- FDA Guidance for Safety Reporting: Part 3 -Other Safety Reporting Issues
- Introduction
- FDA Protocol Requirements
- FDA Protocol Content
- ICH Protocol Content: Part 1 - General Information
- ICH Protocol Content: Part 2 - Background and Trial Objectives
- ICH Protocol Content: Part 3 - Trial Design
- ICH Protocol Content: Part 4 - Selection and Withdrawal of Subjects
- ICH Protocol Content: Part 5 - Treatment of Subjects and Assessment of Efficacy
- ICH Protocol Content: Part 6 - Assessment of Safety and Statistics
- New Protocols: Part 1
- Revised Protocols: Part 1
- Introduction: Part 1
- FDA Investigator Brochure Requirements: Part 1
- FDA Investigator Brochure Requirements : Part 3 - Informing Investigators
- Example IB Table of Contents
- Introduction
- Essential Documents: Part 1
- Investigational New Drug Application
- Statement of Investigator
- FDA Bioresearch Monitoring Program: Part 1
- Penalties
- Documents to be Present Pre-Study
- Documents to be Added During the Study
- Documents to be Added Post-Study
- Glossary
- Useful Documents
Our GCP certified customers


Good Clinical Practice (GCP) training is a vital educational programme designed to arm researchers and clinical trial professionals with essential knowledge of ethical and scientific standards. These standards are crucial for executing high-quality clinical trials. The training encompasses the globally acknowledged guidelines set forth by the International Council for Harmonisation (ICH).
The key objectives of GCP training include:
- Safeguarding the rights, safety, and welfare of human participants
- Upholding the accuracy and reliability of data collected during clinical trials
- Fostering uniform, superior practices across all facets of clinical research
Whitehall Training's Good Clinical Practice Course thoroughly explores these critical areas. Our comprehensive programme equips learners with a robust understanding of GCP principles and their practical implementation in real-world clinical research scenarios. By completing this course, participants gain the necessary skills to conduct clinical trials that meet the highest standards of ethical and scientific rigour.
Absolutely. For those involved in clinical trials, GCP certification isn’t just valuable—it’s essential. But even if you’re not directly participating in trials, obtaining GCP certification offers numerous benefits:
- It demonstrates your commitment to upholding global research standards
- Your research gains added credibility and quality assurance
- You’ll be better equipped to safeguard the rights and wellbeing of study participants
- Your career opportunities in the clinical research sector may expand significantly
Our Whitehall Training Good Clinical Practice Course goes beyond mere certification. We provide you with practical, hands-on knowledge that you can immediately apply in your professional endeavours. By mastering GCP principles through our course, you’ll be well-prepared to navigate the complexities of clinical research with confidence and expertise.
Good Clinical Practice (GCP) certification is crucial for a broad spectrum of individuals working in clinical research:
- Lead Researchers and Co-investigators: These are the primary and supporting scientists responsible for overseeing and conducting trials at research facilities.
- On-site Trial Team: This includes study coordinators, research nurses, and other personnel involved in the day-to-day management of clinical trials.
- Trial Sponsors and Research Organisations: Professionals who manage the overall planning, commencement, and documentation of clinical studies.
- Regulatory Bodies: Officials tasked with supervising and assessing trial compliance with established standards.
- Ethics Committees: Groups responsible for reviewing and approving proposed trial protocols to ensure ethical conduct.
- University and Research Centre Staff: Individuals ensuring that institutional research aligns with international benchmarks.
- Researchers Funded by National Health Organisations: All scientists and support staff engaged in publicly funded clinical trials.
Our comprehensive GCP course is designed to meet the needs of this varied audience, offering both universal principles and role-specific guidance. Additionally, it serves as an excellent resource for those aiming to enhance their research capabilities and refine their approach to clinical trial operations. The Whitehall Training Good Clinical Practice Course provides tailored content to address the unique requirements of each of these professional groups, ensuring that all participants gain the knowledge necessary for their specific roles in the clinical research process.
Our Good Clinical Practice (GCP) course is designed to provide comprehensive coverage of the ICH-GCP (E6-R2) international guidelines, ensuring you meet the necessary training requirements for participation in international clinical trials. We offer this course in multiple languages to cater to a diverse audience.
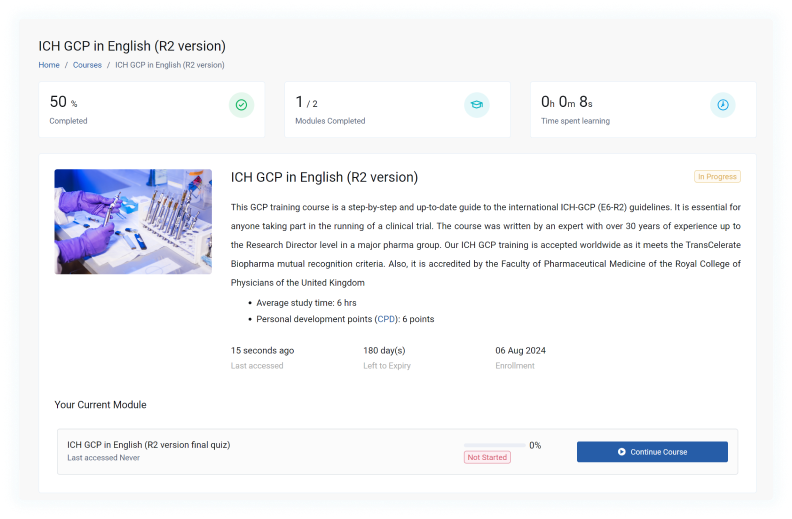
This course serves as a detailed, step-by-step guide to the most recent ICH-GCP (E6-R2) guidelines, making it an indispensable resource for anyone involved in clinical trial management. The content has been meticulously crafted by an industry veteran with over three decades of experience, including a tenure as Research Director at a leading pharmaceutical company.
We’re proud to offer a course that’s accredited by the Faculty of Pharmaceutical Medicine of the Royal College of Physicians of the United Kingdom. This accreditation underscores the quality and relevance of our training material. To accommodate our global learners, we’ve made the course available in ten languages: English, German, Bulgarian, French, Italian, Japanese, Polish, Portuguese, Russian, and Spanish. Additionally, we’ve developed region-specific versions tailored to the regulatory frameworks of Australia, the UK, the US, France, Germany, and Latin America.
Our course stands out for its user-friendly design and clear visual presentation. This format allows for easy navigation and reference to the ICH-GCP E6 document. Drawing from the author’s extensive industry experience, the course offers practical insights into the application of GCP principles.
Upon completion, participants can earn 6 Continuing Professional Development (CPD) points, further enhancing the value of this training programme.
Indeed, our GCP course has received certification from the Faculty of Pharmaceutical Medicine at the Royal College of Physicians. This prestigious body, established in 1989, is renowned for its role in setting stringent research standards and serves as the professional membership organisation for pharmaceutical physicians across the United Kingdom.
The certification bestowed upon our course is a testament to its quality and relevance. It signifies that our programme meets exacting industry and academic criteria, providing you with a qualification that is widely acknowledged and respected within the field. By completing this certified course, you can be confident that you’re receiving training that aligns with the most current and rigorous standards in pharmaceutical research and practice.
The price of GCP certification can fluctuate based on several key factors:
- Endorsement: Has the course received approval from official bodies?
- Validity: Does the training meet ICH standards, allowing researchers to engage in global clinical studies?
- Content quality: Is the material current and authored by an industry expert?
- Duration of access: For how long can students utilise the course materials?
Our Whitehall Training GCP course is priced at £79, reflecting its high value across these areas:
- Endorsement: The Royal College of Physicians has accredited our course, awarding it 6 CPD points.
- Validity: Upon completion, researchers are equipped to participate in clinical trials, in line with ICH E6(R2) guidelines.
- Content quality: Lucy Parker, our GCP specialist with over ten years’ experience leading research at major institutions like the NHS, has crafted the course content.
- Duration of access: We support ongoing professional development by offering unlimited access to course materials.
For group purchases, we offer a 10% discount when buying 5 licences at checkout. If you’re interested in larger group discounts, please reach out to our team for a tailored quote.
Indeed, some free GCP training options can be found online. However, it’s important to be aware of their potential drawbacks:
- The content may be of lower quality, lacking accreditation and potentially outdated
- These courses typically don’t offer official certification, which is often required for conducting clinical research
Our GCP course offers a comprehensive exploration of the essential principles and practices required for conducting ethical and scientifically robust clinical trials. With a curriculum that caters to both newcomers and seasoned professionals, the programme is structured to accommodate various levels of expertise.
The course delves into a range of crucial subjects, including:
- The origins and fundamental tenets of GCP
- Key stakeholder duties: investigators, sponsors, and monitors
- Ethics in clinical trials and obtaining informed consent
- Creating and adhering to trial protocols
- Managing safety reports and adverse events
- Ensuring data quality and integrity
- Navigating regulatory landscapes and authority interactions
- Maintaining crucial documentation and records
- Proper handling of investigational medicinal products
- Best practices in site management and monitoring
To ensure an engaging and effective learning experience, we employ a variety of interactive e-learning techniques, such as:
- In-depth educational content
- Authentic case studies and situational analyses
- Engaging knowledge assessments and quizzes
- Practical illustrations and industry-leading practices
- Reflective exercises and real-world applications
This carefully crafted approach ensures that participants not only grasp the theoretical aspects of GCP but also gain practical insights that can be directly applied in their professional roles.
Securing your Good Clinical Practice certificate is a simple, two-stage procedure:
- Work through the interactive educational content of the course.
- Successfully complete the online assessment at the end.
Feeling apprehensive about the GCP test? There's no need to worry. The examination is merely a formality to confirm your readiness for research participation. In the unlikely event that you don't pass on your first attempt, you can easily brush up on any areas you're unsure of using our comprehensive resource library, and then have another go at the exam.
Our Whitehall Training Good Clinical Practice Course is designed to make this process as smooth and informative as possible, ensuring you're well-prepared for both the exam and your future role in clinical research.
Our Good Clinical Practice course is structured to ensure participants not only absorb the material but can also implement it effectively in real-world clinical research environments. To achieve this, we've incorporated various evaluation methods throughout the learning journey:
- Continuous Learning Checks: As you progress through the modules, you'll encounter interactive quizzes and practical scenarios. These elements serve to reinforce key concepts and allow you to measure your understanding along the way.
- Comprehensive Final Evaluation: The course concludes with an in-depth assessment that thoroughly examines your grasp of GCP principles and practices. This evaluation covers all major areas from the course, including:
- Ethical considerations within clinical studies
- Regulatory compliance and requirements
- Responsibilities and roles in clinical trials
- Quality management and data integrity
- Adverse event handling and safety reporting
- Real-world Application: Some questions in the final evaluation are crafted to test your ability to apply GCP principles to realistic clinical trial situations.
To ensure you're fully equipped to conduct trials, successfully completing the final evaluation is necessary to obtain your GCP certification.
We understand that everyone learns at their own pace, which is why you can take the final evaluation as many times as needed. This approach ensures that all learners can achieve the required standard and become GCP qualified.
Our Good Clinical Practice (GCP) course is tailored to accommodate a broad spectrum of professionals engaged in clinical research. Whilst prior knowledge of clinical research can be advantageous, it's not essential for enrolment. We've carefully crafted the course content to suit various levels of expertise and different roles within the clinical trial field.
This training programme is particularly beneficial for:
- Clinical Research Coordinators
- Principal and Sub-Investigators
- Research Nurses
- Clinical Trial Managers
- Data Managers and Biostatisticians
- Regulatory Affairs Specialists
- Quality Assurance Experts
- Ethics Committee Members
- Pharmacists involved in clinical studies
- Sponsor and Contract Research Organisation (CRO) staff
The course is suitable for both newcomers to clinical research and seasoned professionals seeking to update their knowledge. It offers a comprehensive overview of GCP principles and their practical implementation in clinical trials. The content is structured to ensure that learners at all levels can grasp and apply the concepts effectively, making it an ideal choice regardless of your current level of experience in the field.
Indeed, our Good Clinical Practice course is fully available via the internet, providing learners with unparalleled convenience and adaptability. This digital format offers numerous benefits:
- Personalised learning speed: Students can navigate through the course content at a rhythm that best suits their individual needs and timetable. This approach fosters a more thorough understanding of the material without the constraints often associated with traditional classroom settings.
- Round-the-clock availability: The course can be accessed at any time, from any internet-connected device. Whether you're at your workplace, in the comfort of your home, or even whilst on the move, the course materials are always at your fingertips.
The International Council for Harmonisation, or ICH, plays a crucial role in shaping the landscape of pharmaceutical research and development worldwide. This organisation is at the forefront of establishing globally recognised guidelines, including those for Good Clinical Practice (GCP). Here's what you need to know:
- ICH acts as a collaborative platform, uniting regulatory bodies and pharmaceutical industry experts.
- It develops internationally accepted standards that govern the conduct of clinical trials.
- The ICH GCP guidelines are designed with two primary objectives: safeguarding trial participants and ensuring the reliability of clinical data.
- These guidelines undergo regular revisions to stay current, with ICH GCP E6(R2) being the most recent iteration.
Adhering to these ICH guidelines is non-negotiable for anyone involved in clinical research. That's precisely why we've crafted our Good Clinical Practice course. We provide comprehensive coverage of all 13 fundamental ICH GCP principles, equipping you with the knowledge and skills necessary to conduct research that meets stringent global requirements. Our aim is to ensure you're fully prepared to navigate the complexities of clinical trials in accordance with these internationally recognised standards.
ICH Good Clinical Practice E6 (R2) represents the latest iteration of the Good Clinical Practice guidelines, published in 2016 by the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. This update marks a significant progression in GCP standards, adapting to the evolving landscape of clinical research.
It's essential for clinical research professionals to be well-versed in ICH GCP E6 (R2) for several reasons:
- It sets the current worldwide benchmark for conducting ethical and scientifically rigorous clinical trials.
- Regulatory bodies across the globe often mandate adherence to these guidelines.
- It plays a crucial role in safeguarding study participants and ensuring the integrity of trial results.
- Many research institutions and pharmaceutical companies expect their teams and collaborators to be knowledgeable about and compliant with these updated standards.
The Whitehall Training Good Clinical Practice Course offers comprehensive coverage of ICH GCP E6 (R2). Our programme ensures that learners gain a thorough understanding of these revised guidelines and can effectively implement them in their clinical research endeavours. By focusing on the most up-to-date standards, we equip participants with the knowledge needed to excel in the current clinical research environment.
The International Council for Harmonisation (ICH) Good Clinical Practice (GCP) guidelines are founded on 13 essential principles that serve as the cornerstone for ethical and scientific standards in clinical research. These crucial principles encompass:
- Conducting research ethically
- Ensuring benefits surpass risks
- Safeguarding participants' rights and wellbeing
- Providing sufficient supporting evidence
- Developing scientifically robust protocols
- Obtaining IRB/IEC approval
- Ensuring qualified medical oversight
- Engaging competent investigators
- Securing informed consent
- Maintaining precise data documentation and reporting
- Upholding confidentiality
- Adhering to good manufacturing practices for investigational products
- Implementing quality assurance systems
Our Whitehall Training Good Clinical Practice Course offers comprehensive instruction on these principles, equipping you with the knowledge to effectively implement them in practical clinical research scenarios. Through our course, you'll gain a thorough understanding of how these principles shape the landscape of clinical trials and contribute to the integrity of research outcomes.